By Kevin Sang, Uasin Gishu
Antimicrobial Resistance (AMR) is a growing global health threat, and Kenya is not immune to its dangers. AMR occurs when bacteria, viruses, fungi, and parasites evolve to resist the drugs designed to eliminate them.
This makes common infections harder to treat and increases the risk of disease spread, severe illness, and death. In Kenya, the misuse of antibiotics in both humans and animals has accelerated the rise of drug-resistant microbes, leading to devastating consequences for public health and the economy.
The Growing Threat of AMR in Kenya
AMR is not just a medical issue; it threatens food security, economic development, and national health systems. In Kenya, like many developing countries, the over-the-counter sale of antibiotics without proper prescriptions is common.
Many people take antibiotics for viral infections like the flu, which antibiotics cannot treat, or stop taking them once they feel better without completing the prescribed dose. These practices allow bacteria to survive and adapt, eventually rendering the antibiotics ineffective.
According to the World Health Organization (WHO), by 2050, drug-resistant infections could cause 10 million deaths annually worldwide, with the most severe impacts expected in Africa. In Kenya, we are already witnessing increasing cases of drug-resistant tuberculosis (TB), malaria, and bacterial infections like pneumonia.
AMR in Animals and Crops: A Silent Path to Human Infection
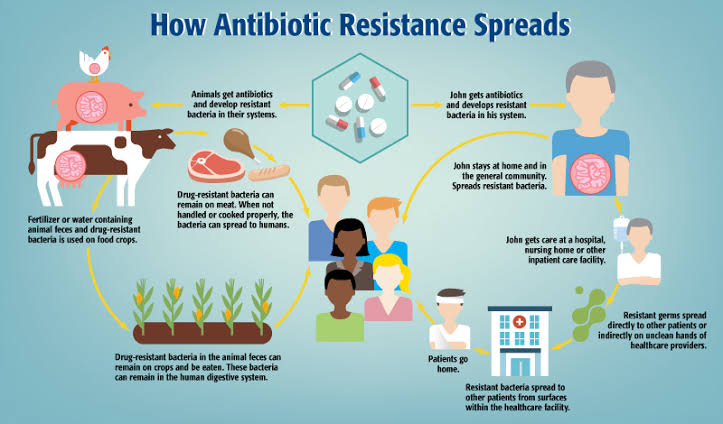
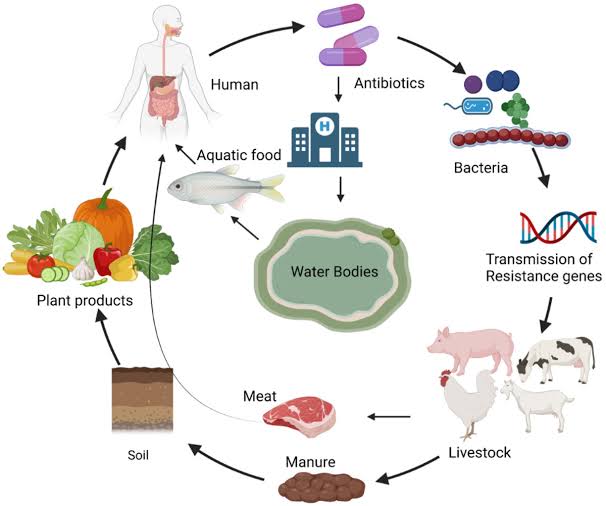
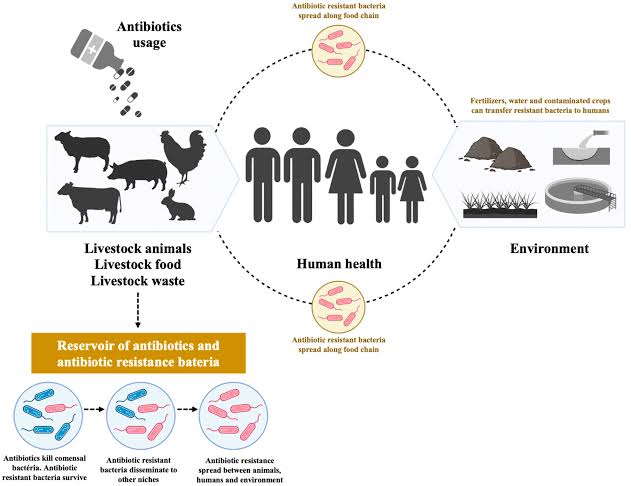
AMR doesn’t just develop in humans. The overuse of antibiotics in agriculture, particularly in livestock and crop production, also plays a significant role.
In Kenya’s livestock sector, antibiotics are often administered to healthy animals to promote growth and prevent disease, rather than treat infections. Similarly, in crop farming, antibiotics are used to prevent plant diseases.
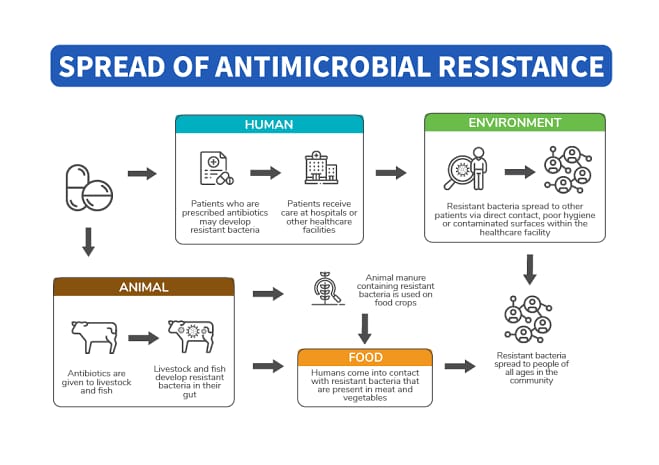
When animals and crops are treated with antibiotics excessively, resistant bacteria can emerge and survive in food products. These bacteria are then transferred to humans through consumption of contaminated food or contact with the environment.
For instance, consuming meat or milk from animals raised with antibiotics can expose people to resistant bacteria. In this way, the careless use of antibiotics in agriculture threatens not only food safety but also human health.
AMR Reaching the Public
AMR spreads through multiple channels. In Kenya, where access to clean water and sanitation is a challenge in many rural and urban areas, resistant bacteria can spread easily through water systems and soil, infecting people who have no direct contact with the animals or plants from which the bacteria originated.
Moreover, Kenya’s informal food markets and the widespread use of untreated water for irrigation increase the risk of AMR transmission.
Hospitals, too, are breeding grounds for resistant bacteria, especially when infection control measures are inadequate. Many healthcare facilities in Kenya lack the necessary resources for strict infection prevention, contributing to the rise of hospital-acquired infections that are difficult to treat.
What Can Be Done?
Kenya must take serious action to prevent the further spread of AMR. Awareness is key, as many people remain unaware of the long-term consequences of misusing antibiotics. Health professionals, the public, farmers, and policymakers all have roles to play in combating AMR.
Use Antibiotics Responsibly: People should only take antibiotics when prescribed by a qualified healthcare professional. Patients must complete the full course of medication, even if they start feeling better, to ensure all bacteria are eliminated and do not become resistant.
Strengthen Regulations: Kenya needs to enforce stricter regulations on the sale of antibiotics. Pharmacists should require prescriptions before dispensing antibiotics, and the government must tighten controls on antibiotic use in agricultur
Improve Infection Prevention: Hospitals should be equipped with better infection control measures to reduce the spread of resistant bacteria. This includes improving sanitation, ensuring access to clean water, and promoting hand hygiene.
Promote Research and Surveillance: The Kenyan government should invest in research on AMR to better understand its prevalence and spread. Surveillance systems can help track resistant infections and guide interventions more effectively.
Raise Public Awareness: Educational campaigns targeting both the public and farmers should emphasize the dangers of AMR and promote the responsible use of antibiotics.
In conclusion, Kenya is at a critical point in the fight against AMR. Without immediate and coordinated action, resistant infections could become the leading cause of death and disability. We must prioritize responsible antibiotic use in both humans and animals, strengthen our healthcare system, and invest in research to curb this silent but growing threat. If we fail to act, we risk reversing decades of medical progress and jeopardizing the health of future generations.